On World Tuberculosis Day, lessons for COVID-19
Inuit are united in our determination to eliminate TB in our communities. Today is World TB Day, and as we face a new pandemic in COVID-19, we know that the same conditions of everyday life that leave Inuit at high risk for TB also increase our risk for COVID-19. These conditions are the social story behind the clinical stories of both TB and COVID-19. Facing a new pandemic makes bold action to build better health systems and improve our conditions of everyday life more urgent than ever.
While Nunavut does not yet have any confirmed cases of COVID-19, we know that Inuit experience the highest rates of TB of any population in Canada. Inuit know too well that infections and inequalities are closely linked. TB closely reflects patterns of social inequity in housing, nutrition, poverty, and access to health care. It is likely that COVID-19 will follow similar patterns, as equity gaps in housing, nutrition, and other social determinants of health leave Inuit at higher-risk for both infections than other populations.
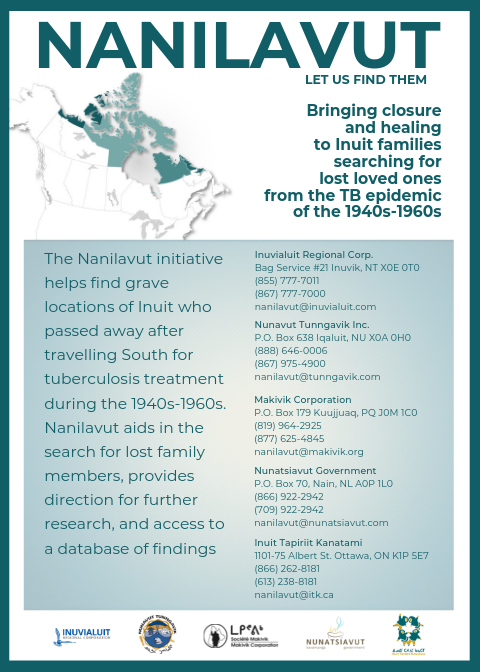
On March 8, 2019, the Government of Canada apologized to Inuit for the management of the tuberculosis epidemic from the 1940s to the 1960s. That apology was a long time coming and signaled a step towards healing and reconciliation. On March 23, 2018, the Government of Canada and Inuit Tapiriit Kanatami committed to eliminating TB across Inuit Nunangat by 2030, and reducing active TB by at least 50 per cent by 2025.
TB is caused a bacteria called mycobacterium tuberculosis. People can become infected with TB by inhaling air that has TB germs in it, but not through physical contact or by sharing dishes or clothes. Once inhaled, TB bacteria can stay latent (not active) in the body for several years before causing TB disease. TB is entirely preventable and treatable. TB screening is important because it protects you, your family and your community. Visit your local health centre for screening.
COVID-19 is a new disease that has not been previously identified in humans. It is part of a family of viruses (coronaviruses) that are a common cause of illness in people and animals. People can become infected by COVID-19 by inhaling air that has COVID-19 germs in it, by touching surfaces where droplets have landed and then touching their face, mouth or nose, or by physical contact such as handshaking, hugging or kissing. People can be infected with COVID-19 for up to 14 days before symptoms arise.
COVID-19 is not currently treatable, however, social-isolation and self-monitoring can help reduce the spread of the virus. Stay home, wash your hands often and make sure to self-isolate for at least 14 days after returning from travel anywhere in Canada. If you spot any of the symptoms of COVID-19 such as a fever, cough or trouble breathing, self-isolate and contact your local health centre immediately.
We continue to call on our governments to take decisive action to eliminate TB and to prevent and control COVID-19. To achieve these shared goals, we need ongoing political commitments to bring about health equity for Inuit. Together, we can learn from past mistakes, empowering Inuit excellence and leadership in making our own communities more resilient and healthy.
Learn more about tuberculosis from the Public Health Agency of Canada, and from the Government of Nunavut.
Learn more about COVID-19 from the Public Health Agency of Canada, and from the Government of Nunavut.
Some statistics on why Nunavut is vulnerable to TB and COVID-19:
- Housing: 56 per cent of Inuit in Nunavut live in crowded homes.
- 32 per cent of Nunavut Inuit have housed a temporary resident (hidden homeless) in the past year.
- Overcrowded housing increases TB risk. It also increases the risk of spreading COVID-19.
- Nutrition: 70 per cent of Nunavut Inuit are food insecure, compared to 8 per cent of other Canadians.
- 1,734 children in Nunavut do not have any food for at least one day each year.
- Poor nutrition increases TB risk. Access to food is also a concern during the spread of COVID-19, with disruptions to the food chain supply.
- Incomes: Median income for Inuit in Nunavut is $24,768. Median income for non-Inuit in Inuit Nunangat is $84, 139 as of 2018
There are many lessons we can learn from TB to apply to our work on fighting COVID-19. Here are some more facts about TB in Canada, Inuit Nunangat, Nunavut, and the Qikiqtani Region:
- Canada:
- 4.8/100,000 = the number of new cases per year (incidence rate) of active TB (2016)
- 0.6/100,000 = the number of Canadian-born non-Indigenous population with active TB per year (2016)
- Inuit Nunangat:
- 182.9/100,000 = the overall incidence rate of TB among Inuit living in Inuit Nunangat (2016)
- This number is 300 times the rate of TB among non-Indigenous Canadian-born population
- 182.9/100,000 = the overall incidence rate of TB among Inuit living in Inuit Nunangat (2016)
- Nunavut:
- 181.1/100,000 = the average incidence rate of TB for the years 2006-2016
- Outbreaks have occurred in communities in 2010, 2012, 2014, and 2017.
- In 2017, 11 of 25 communities had active TB cases reported.
- Outbreaks have occurred in communities in 2010, 2012, 2014, and 2017.
- 181.1/100,000 = the average incidence rate of TB for the years 2006-2016
- Qikiqtani Region:
In Nunavut, TB activity is highest in the Qikiqtani Region, with an average of 305.1 new cases of TB per year from 2006-2016.